Wellfie Wednesday Tip #137: Sleep & Pain Sensitivity
/Happy Wellfie Wednesday! Welcome back! This week is brought to you by Patrick (@TheFuelPhysio) and the topic revolves around how sleep can affect your pain sensitivity.
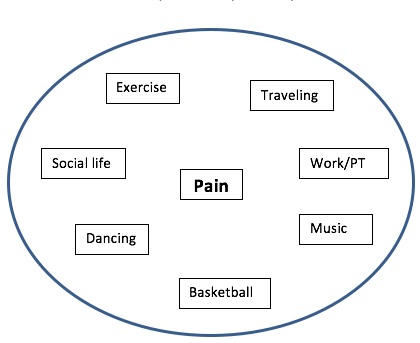
For starters, pain is a very complex thing, especially chronic pain, and it seldom deals with just a physical sensation. Our brain and neurological system controls a lot of it, and it can be a combination of experiences, exposures, and interpretations of painful situations, whether physical or emotional, that contribute to our sensation of pain. Now sleep, the body’s ability to recover, has been discovered to be something that should be of concern when it comes to pain and pain sensitivity.
A recently published study found that individuals with just a single night of sleep deprivation had a 15-30% increase in pain sensitivity, reducing their pain threshold. Meaning there interpretation of a painful stimuli came sooner than if adequate sleep was had the night before. In agreement with sleep playing a role in pain sensitivity, another recent study found that extended sleep could increase an individual’s pain threshold.
Both of these studies of course have several limitations, but their findings should still be considered. So if you or someone you know is dealing with pain, getting a better night sleep could be a good start. And I know that’s easier said than done for most. Check out this resource by the American Academy of Sleep Medicine for some helpful tips to improving your sleep.
Thanks for all of the support, be sure to post your pictures this week and tag the WW crew members in your post (@TheFuelPhysio, @Eric_in_AmERICa, @FreestylePhysio, @DianaKlatt) and keep the wave of healthy change going!
- WW Crew
Krause, A. J., Prather, A. A., Wager, T. D., Lindquist, M. A., & Walker, M. P. (2019). The pain of sleep loss: A brain characterization in humans. Journal of Neuroscience, 2408-18.
Simonelli, G., Mantua, J., Gad, M., St Pierre, M., Moore, L., Yarnell, A. M., ... & Capaldi, V. F. (2019). Sleep extension reduces pain sensitivity. Sleep medicine, 54, 172-176.